Last time, we discussed the concept of telehealth and the ways it’s applied to achieve better, cost-effective patient outcomes in the United States. In this article, the spotlight is on the technical features of usable, future-proof custom telehealth software solutions that help drive a successful telehealth transition.
More often than not, healthcare providers dive into telemedicine without realizing there’s no one-size-fits-all solution. Customized telehealth solutions are essential to meet the unique needs of each healthcare provider.
Kristi Henderson, a healthcare executive with decades of telehealth implementation under her belt, warns first-timers against trying to shoehorn a popular platform into the established continuum of care. On the other hand, bringing on board sufficient technical expertise to scope, develop and modify the solution as necessary is a great way to have your specific clinical needs met.
The checklist below outlines some of the key aspects to keep in mind while envisioning and planning out your custom healthcare solution.
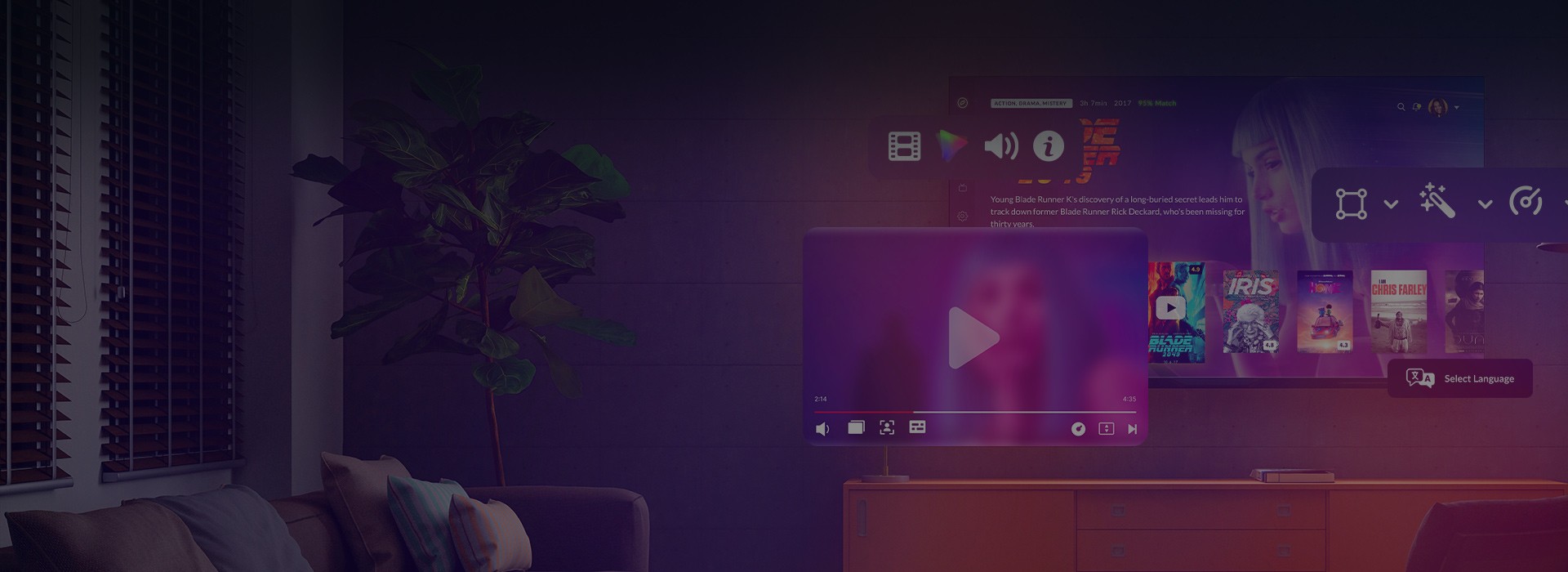
UX & UI

Enthusiastic adoption of any telehealth initiative hinges on UX.
If users are not comfortable with the technology from the get-go, little can be done to persuade them to switch to virtual care.
Make sure your tech team understands UX from the provider’s and the patient’s perspectives equally well.
Workflows need to stay familiar and the UI intuitive both on desktop and mobile to shorten the adaptation period and mitigate training costs. A good example of such an approach is a virtual waiting room that engages the patient before the doctor is available to take their call.
Accessibility

Accessibility is an important issue for any technology, but for applications that are meant to be used by sick, elderly, or disabled people it’s critical.
Is your web solution screen reader-friendly? Does your RPM (Remote Patient Monitoring) package provide for patients with nerve damage or otherwise diminished reflexes? How about enabling a medically qualified ASL interpreter to assist a hearing-impaired patient during a live video conference?
At this stage, cooperation is key: urge your tech team to work closely with a subject-matter expert from your clinical staff to determine what assistive technologies and accessibility settings your solution will need.
Collaboration Capabilities

A well-rounded telehealth solution should provide means of collaboration and data exchange to enhance consults between caregivers and make doctor-patient communication more interactive.
Here, the WebRTC technology delivers on both fronts. A WebRTC module can be embedded directly into your telehealth solution to enable plugin-free video and audio calls from any connected browser or mobile device.
On top of that, the technology comes with effective collaboration features, including screen- and file-sharing, as well as on-screen annotations.
Data Confidentiality and Security

Under the HIPAA Privacy Rule, covered entities — health plans, health care clearinghouses, and certain health care providers — are obligated to protect patient health information (PHI). Thus, information security is a priority for every telehealth program.
Keep in mind that an HIPAA-compatible platform must provide secure electronic exchange of any PHI, including protection from third party interference in video conferencing and prevention of medical identity theft in the cloud.
Some of the industry’s time-tested measures to address such issues would include firewalling, TLS-based network communication security, two-factor authentication for remote PHI access, strong data encryption with trusted algorithms like AES-256, intrusion detection and alerting, as well as regular penetration testing and vulnerability scanning.
Data Transmission

To be as reliable as face-to-face visits, online consultations need to deliver high-quality, low latency video and audio.
At the same time, providers cannot count on all patients to have access to a high-speed internet connection.
This is why your solution should make allowance for low bandwidth in remote locations and poor network signal on mobile devices.
One of the ways to address the issue is to rely on audio and video transcoding to ensure the best possible media experience with a given bandwidth and network capacity.
Data Interoperability

Lack of all-encompassing data interoperability is a major stumbling block for American telehealth.
Legacy EHRs and EMRs aren’t always integration-friendly, and adapting them to the new types of data that come with telehealth (video examinations, readings from wearables in RPM, patient-generated medical images, informal health information, etc.) can be a real chore.
Allocate time and effort to data governance. Have your tech team establish all the data sources you want included into your solution, aggregate and standardize the data, and map out an integrated workflow.
The job is a meticulous one, but the reward for breaking down data silos is a holistic picture of delivered care, streamlined interdepartmental cooperation, and better informed clinical decisions across your organization.
Big Data and BI

A powerful analytics module is a great feature that can bring both immediate and long-term benefits to your telehealth program. E.g. in RPM, early detection of adverse trends and small changes in a patient’s vitals helps manage complex cases with multiple chronic conditions.
At the same time, a rigorous analysis of your chosen ROI metrics can produce actionable insights into the progress of your telehealth strategy as a whole.
While BI is a common ingredient in telehealth programs, big data is still largely untapped. IBM reports that 80% of digital medical data comes in an unstructured format, making it as good as useless for large-scale processing.
That doesn’t mean, however, that your organization should shrug off the potential of big data implementation. This much-talked-about technology is poised to deliver a profound impact on population health by unlocking the value of routinely collected data for epidemiological research, clinical trial design, genomics, and more.
The Full Picture
It must be noted that specialized technology is just the tip of the telehealth adoption iceberg. There are multiple issues that demand attention before the program truly gets off the ground: full stakeholder buy-in, legal constraints, comprehensive staff training, limited awareness among the target audience, and so on.
In the absence of definitive national guidelines, first-timers turn to local telehealth resource centers and other organizations’ best practices for advice. Some providers prefer to address a specific pain point with an ad hoc standalone solution, while others favor the scalability of enterprise-wide platforms.
The market is ripe for cost-effective and time-saving offers. Whichever combination of tech, strategy, and budgeting underpins your program, commitment to telehealth will give your organization the competitive edge it needs to retain and expand your patient base.